Prolapse Repair
Prolapse repair using patient's own tissue
For a patient with pelvic organ prolapse, there are THREE management options.
a. OPTION 1: Conservative management. Do nothing for now. Prolapse does NOT suddenly develop in a few months or in 1 year. Prolapse develops over many years (e.g. 2-10+ years).
b. OPTION 2: Trial of pessary management
c. OPTION 3: Surgery for prolapse. The first line of surgical treatment is to use the patient's OWN tissue for prolapse repair. The advantage of using a patient's own tissue is that NO foreign body (no synthetic mesh) is used, so the patient avoids all the complications associated with synthetic mesh.
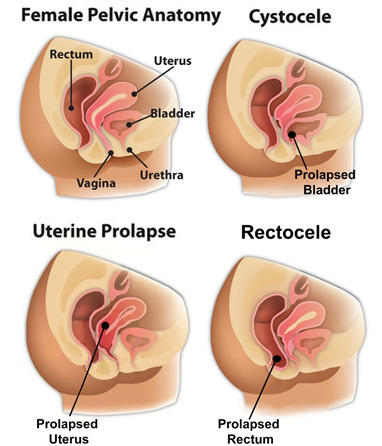
The vaginal canal is divided into THREE compartments of prolapse
a. Cystocele (aka bladder prolapse) is defined as prolapse of the anterior compartment.
b. Uterine prolapse is defined as prolapse of the apical compartment
c. Rectocele is defined as prolapse of the posterior compartment.
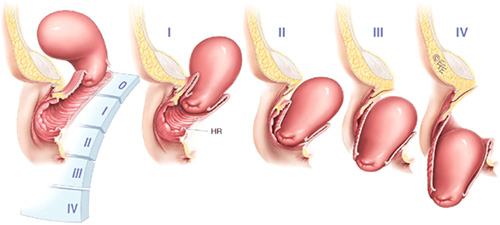
For each COMPARTMENT, there are FOUR stages of prolapse
For instance, there are four stages (I-IV) of uterine prolapse. Also, four stages (I-IV) of bladder prolapse and four stages (I-IV) of a rectocele. The example below focuses on Stage I-IV of uterine prolapse.
a. Stage I. Mild uterine prolapse. The uterus falls halfway down the vaginal canal.
b. Stage II prolapse. MODERATE uterine prolapse. The uterus falls to the opening of the vaginal introitus (aka opening).
c. Stage III uterine prolapse. SEVERE prolapse. The uterus falls outside the opening of the vaginal introitus, between 2-5 cm outside the vaginal introitus.
d. Stage IV uterine prolapse. SEVERE prolapse (aka Complete procidentia). The uterus falls 6-8 cm outside the opening of the vaginal introitus.
INDICATION for prolapse surgery.
a. For Stage I prolapse, 30-50% of women who have had vaginal deliveries have a MILD stage I prolapse. The treatment option is ALWAYS conservative management. Do nothing.
b. For Stage II prolapse, if the patient is ASYMPTOMATIC, then conservative management is the best options. If the patient is SYMPTOMATIC, then the next step would be to consider pessary management or surgical intervention.
c. For Stage III and Stage IV prolapse, conservative management is NOT an option. The next step will be to consider pessary management or a surgical intervention.
d. OVERALL, if surgery, the plan would be to fix all the compartments of prolapse or conservative management. For instance, if a patient has a Stage II bladder prolapse, Stage II uterine prolapse, and a Stage II rectocele, the patient will have TWO OPTIONS:
OPTION 1: Conservative management.
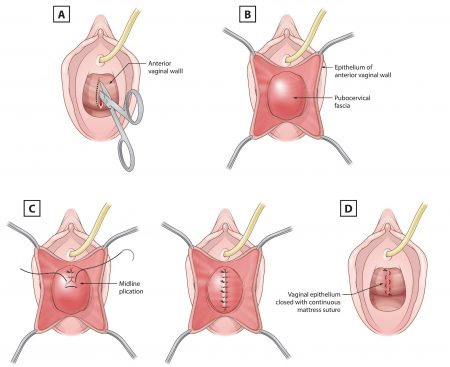
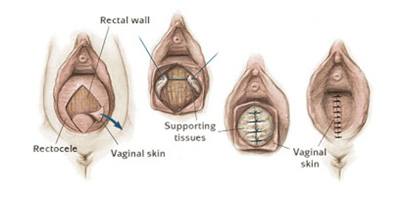
OPTION 2: Prolapse repair which would include a hysterectomy (e.g. LAVH), bladder repair (aka anterior colporrhaphy), a colpopexy procedure (aka apical suspension to the high uterosacral ligaments), and a rectocele repair (aka posterior colporrhaphy). The entire prolapse repair would be performed using the patient's OWN native tissue. No synthetic mesh.
Anterior compartment repair (aka cystocele repair or bladder repair)
Posterior compartment repair (aka rectocele repair)
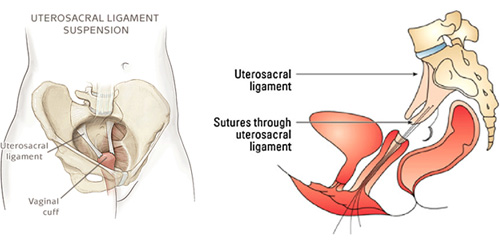
Apical suspension repair (aka HIGH UTEROSACRAL ligament suspension)
Surgical limitations of the prolapse repair.
The primary limitation of the prolapse repair is the STRENGTH of the patients underlying FASCIAL TISSUE. I will not be able to determine the strength of the patient’s own tissue until intraoperative evaluation at the time of the surgery. The strength of the patient’s own tissue will be good predictor of the durability and longevity of the surgical repair. An analog is that a prolapse (aka TEAR in the patient’s own fascial tissue) is like a TEAR in a pair of pants. When the surgical repair is performed, the surgeon is trying to identify the tear and reapproximate the tear back together.
a. A patient who has STRONG fascial tissue is like a tear in a pair of jeans. Once the tear in sewn back together, the repair should be STRONG and durable
b. A patient who has AVERAGE fascial tissue is like a tear in a pair of khaki pants. Once the tear is sewn back together, the repair should be AVERAGE in strength.
c. A patient who has WEAK fascial tissue is like a tear in a pair of silk pants. Once the tear is sewn back together, the repair is STILL WEAK and there is a higher likelihood of recurrent prolapse in the future
d. OVERALL, a surgeon will not be able to assess the strength and durability of a patient’s tissue until INTRAOPERATIVE examination.
Post op recovery
The two main limitations during the sacral colpopexy procedure are:
a. No heavy lifting (x < 15 lbs.) for 3 months post-surgery
b. Showers only. No baths, no pools, no intimacy, and no soaking in any water for 2 months post-surgery. Overall, each patient heals at their own rate, so each patient needs to listen to her body, with activity as tolerated.
c. Full recovery with return to normal activities in approximately 6 weeks.